Endodontic Diagnosis 11/19/2018
What’s the hardest part of endodontics? Is it access? Instrumentation and obturation? With enough experience, any clinician will tell you that these phases of endodontic therapy become routine. However, what’s not routine and can present a challenge to any practitioner is proper endodontic diagnosis! I emphasize the word proper because not everyone is familiar with the terminology adopted by the American Association of Endodontists.
It should be kept in mind that determining a diagnosis is like putting together a puzzle: there are multiple pieces that are needed for completion. Review of medical history, diagnostic quality radiographs, and clinical examination/ testing are required for interpretation of both a PULPAL and PERIRADICULAR diagnosis. Also- listen to your patient! Many times your patient will tell you what’s happening before your examination begins.
The American Association of Endodontists recognizes the following PULPAL diagnostic terms:
1. Normal Pulp- pulp is symptom free and responds normally to vitality testing
2. Reversible Pulpitis- Subjective and objective findings indicate that the inflammatory response in the pulp should resolve and the pulp return to normal after removal of the etiology. Common etiologies include: exposed dentin(recession), caries, and “high” restorations
3. Symptomatic Irreversible Pulpitis- The inflammatory response in the pulp is irreparable and root canal therapy is indicated. Common symptoms are: spontaneous pain, lingering pain to thermal stimulus
4. Asymptomatic Irreversible Pulpitis- A symptom free pulp of which the vital inflamed pulp is beyond repair and root canal therapy is indicated. These cases typically respond normally to vitality testing. An example of this type of case is visible caries to the pulp of which removal would result in pulp exposure
5. Pulp Necrosis- The tooth/pulp is beyond repair and root canal therapy is indicated. The pulp does not respond to vitality testing (ie, cold and/or EPT). However, CAREFUL of calcified teeth- these teeth typically have a limited response to cold testing and may give a false negative!
6. Previously Treated- Prior endodontic therapy with the canals obturated with a filling material
7. Previously Initiated Therapy- The tooth has been treated with partial endodontic therapy such as pulpotomy or pulpectomy
The American Association of Endodontists recognizes the following PERIAPICAL diagnostic terms:
1. Normal Apical Tissues- No symptoms to palpation and bite stick testing (I typically do not rely on percussion testing- that’s a story for another time), and radiographically the lamina dura and pdl are intact without interruption; no suggestive evidence of apical periodontitis
2. Symptomatic Apical Periodontitis- represents inflammation within the periapical tissues. Symptoms include discomfort with palpation and/or bite stick testing. This may or may not be accompanied with radiographic evidence of apical periodontitis
3. Asymptomatic Apical Periodontitis- this is deterioration of the apical periodontium that is of pulpal origin. There is evidence of apical periodontitis without clinical symptoms
4. Chronic Apical Abscess- an inflammatory reaction of pulpal necrosis with clinical evidence of a sinus tract in the gingival tissues. The area may or may not be symptomatic
5. Acute Apical Abscess- an inflammatory reaction to pulpal necrosis which is characterized by rapid onset, spontaneous pain and swelling. There may or may not be radiographic evidence of apical periodontitis. The key is swelling!
6. Condensing Osteitis- a diffuse radiopaque area at the apex of the tooth which represents a bony reaction to a low- grade inflammatory stimulus
To make an ACCURATE diagnosis, the pulpal diagnosis must be accompanied with a periapical diagnosis.
Two examples with brief scenario are below:
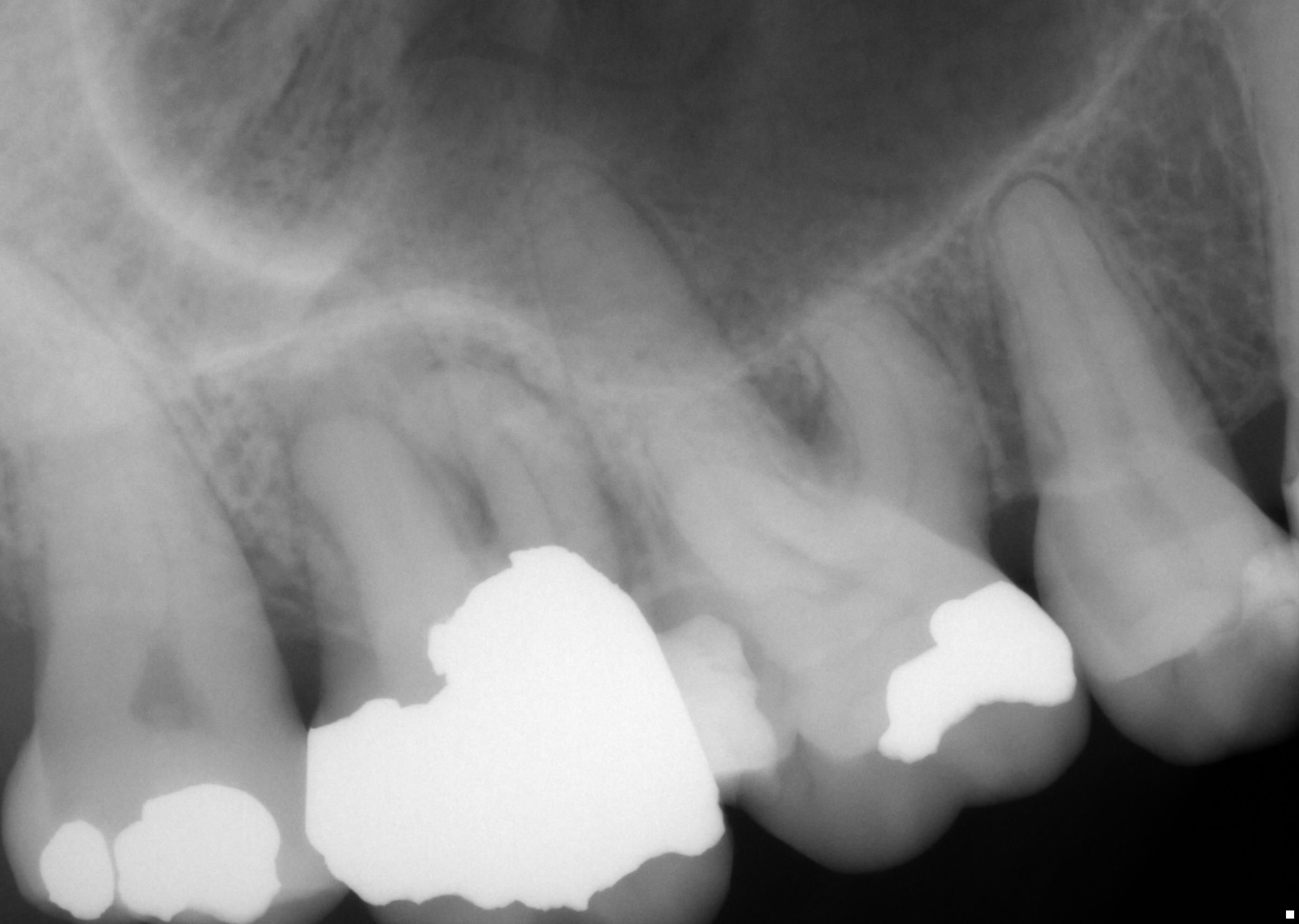
Case 1: Patient presented to our office this past Tuesday with spontaneous pain of 3 days’ duration localized to tooth #2. Her chief complaint was pain mainly upon biting and chewing. No thermal pain reported. Clinical and radiographic findings included: Pain upon bite stick application and palpation tenderness over the buccal root apices. Tooth #2 had no response to cold and EPT vitality testing. Radiographic interpretation yielded the presence of apical periodontitis at the root apices of tooth #2. The diagnosis of tooth #2 is: Pulp Necrosis with Symptomatic Apical Periodontitis. RCT performed without incident.
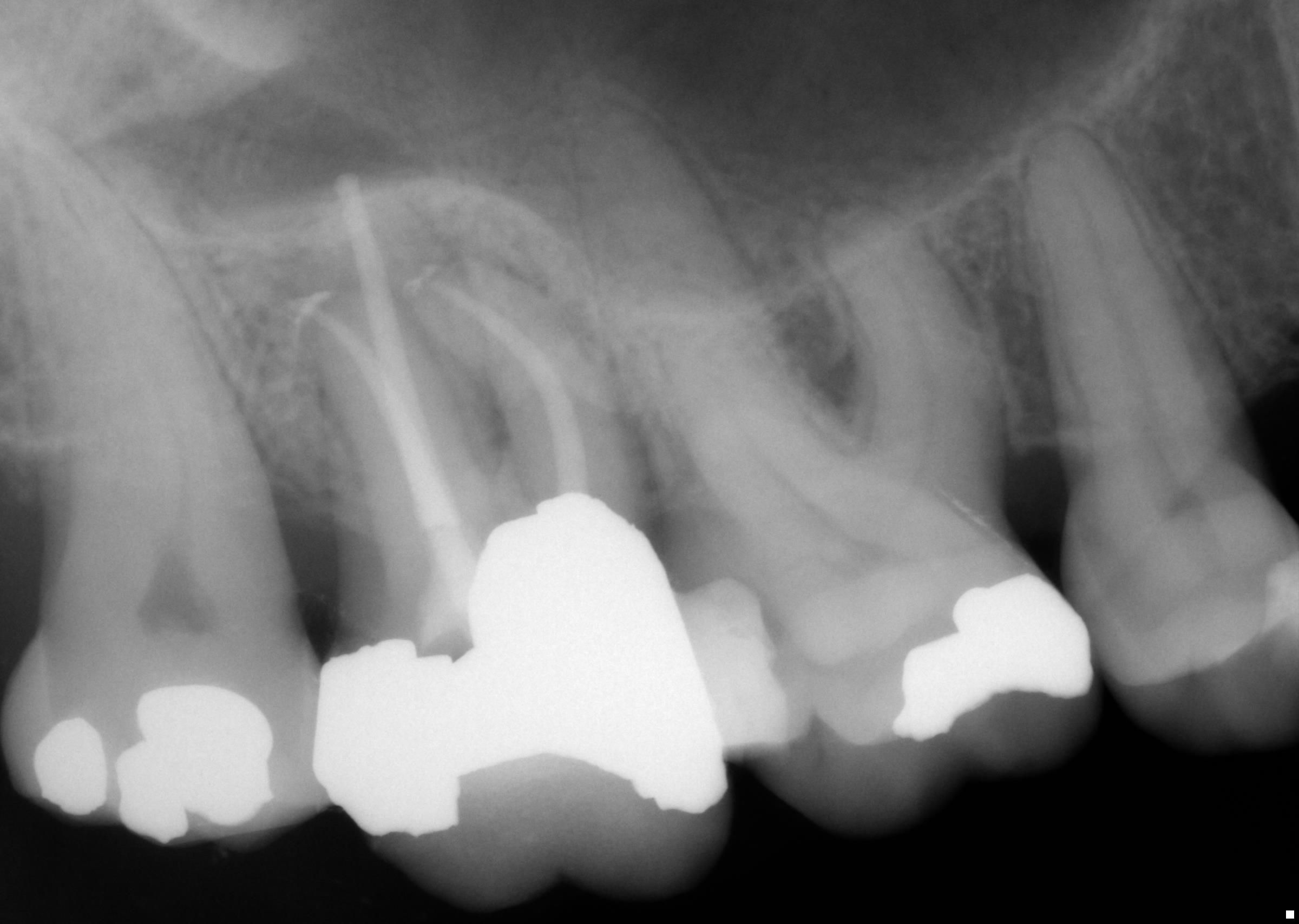
Case 2: Patient presented with “pressure” sensitivity localized to tooth #7. She had reported prior RCT therapy by her dentist. No history of thermal sensitivity; only pain “when pressing” on the gingival tissues. Clinical and radiographic findings included: Visible sinus tract over the apparent apex of tooth #7. She reported discomfort with palpation over the sinus tract and apex tooth #7. Radiographic interpretation yielded prior RCT #7 and a large, diffuse area of apical periodontitis at the apex with extension to the mesial root surface. The diagnosis of tooth #7 is: Previously Treated with Chronic Apical Abscess. Surgical apicoectomy was performed without incident.
Have a wonderful Thanksgiving and until next time,
Jamie
Maxillary Sinusitis 11/12/18
November 12, 2018
Maxillary sinusitis
There exists a strong relationship between dental infections and sinus disease; this was first described in 1943 as maxillary sinusitis of dental origin (MSDO). In fact, it has been reported in the literature that dental infections may account for more than 40% of maxillary sinusitis cases.
MSDO is a broad term which may be caused by many dental etiologies, including periodontal disease, endodontic disease, root fractures, implants, and iatrogenic causes such as dental extractions and over- extruded dental materials. If the etiology is not treated, your patient may suffer from chronic sinusitis infections, ineffective antibiotic regimens, and may see multiple MDs for extensive sinus surgeries.
For the purpose of today’s blog, I will refer to such sinusitis as Maxillary Sinusitis of Endodontic Origin (MSEO). In order to determine if a patient’s perceived “sinus infection” is from endodontic origin, a complete exam must be performed. This includes:
1. Diagnosis
a. Typical endodontic symptoms (ie, hot/cold sensitivity, spontaneous pain) are not often present with MSEO. Usually these teeth are necrotic or present with post- treatment endodontic pathosis (failing root canal).
b. These patients often present with common sinonasal symptoms: UNILATERAL congestion, rhinorrhea, facial pain and/or foul odor.
c.Therefore it is important to pay attention to your patient’s symptoms, distinguish between UNILATERAL or BILATERAL pain, and perform proper vitality testing(s) when indicated.
2. Radiographic Examination
a. Using conventional PA films may be difficult to interpret due to anatomical structures (zygoma, palatal process, maxillary sinus, and buccal cortical plate) which may be superimposed over the roots and apices of the suspect offending maxillary tooth.
b. CBCT imaging has been shown to significantly improve the ability to detect sources of MSE
i. In a study published within the Journal of Endodontics, Low et al. showed that CBCT yielded 34% increase in the detections of apical radiolucent patterns when compared to PA films
ii. CBCT may be able to detect Periapical Mucositis- which is the formation of a “cloudy” expansion into the sinus. This is mucosal edema and coincides with the visible root apices near the sinus.
3. Treatment of MSEO
a. Removal of the irritants which are the cause
i. Root canal therapy, Non- surgical retreatment, surgical retreatment, or extraction
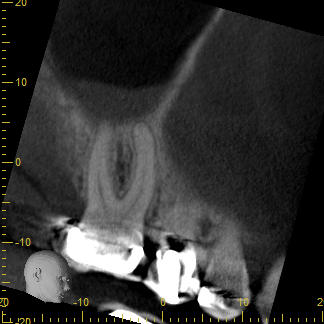
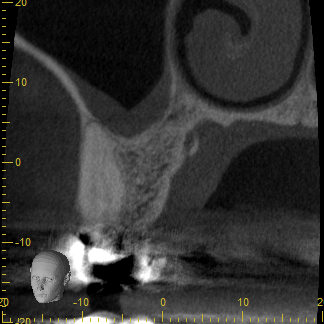
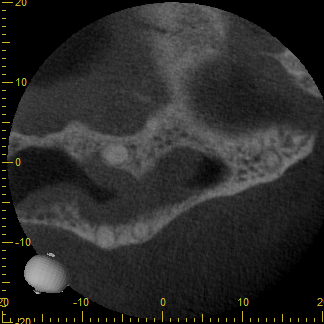
Attached are CBCT images of a patient that I saw this week who presented with a perceived “sinus infection.” She had seen her primary care provider multiple times with a unilateral “pressure headache”, was prescribed antibiotics, and reported that “it never went away.” I diagnosed tooth #3 with a necrotic pulp with symptomatic apical periodontitis, performed RCT, and follow up with the patient provided that her “headaches” went away.
The take home message: Diagnosis is key and many times a perceived “sinus infection” may be dental after all!
Below, from left to right: Sagittal, Coronal, and Axial images from CBCT. Note the proximity of the apices of tooth #3 to the sinus cavity. In addition, note the “cloudy” appearance within the sinus (PAM). This may explain the patient’s unilateral “pressure headaches” and symptomology.
If you wish to discuss more, please call or email me anytime!
Until next week-
Jamie
Proper Patient Follow-up Upon Root Canal Completion 11/05/18
November 5, 2018
Dear Friends and Colleagues:
Words cannot describe how appreciative I am of your support during our transition into Cornerstone Endodontics! My family and I are absolutely thrilled to be a part of the Lincoln dental community.
If you have not visited our newly remodeled website, I strongly encourage you to do so. Karla and our office manager Jenn, worked many hours to design the site and it is now available for you and your patients to use. You can access it here: https://www.cornerstoneendo.com/welcome.html
In addition to assisting your patients, I would like to spend time with you each week via my personal “blog”- which can be accessed through our website and Facebook page. The blog will include topics of interest and some of my personal thoughts, which will be shared each Monday. Also included will be a “case of the week” that’s performed by either Karla, Jeri, or myself.
Should you have any topics of interest, you are welcome to call or send an email my way at drjamie@cornerstoneendo.com
Without further adieu, a question I generally get asked by patients once treatment is completed is
“When do I see my dentist next and does this tooth crown need a crown?”
When I answer this question, I typically like to back my response with literature and evidence based dentistry. Your patient will be told to have the permanent seal placed over the gutta percha within 30 days after RCT completion. Why 30 days? Khyat et al., published in the Journal of Endodontics, showed the bacteria which live in saliva can fully penetrate the obturated root canal system in under this time frame. While we like to pack a temporary restoration into the access cavity, we feel that it is in your patients’ best interest to have the access permanently restored within 30 days after completion of treatment, albeit the tooth may still be tender.
Posterior molars which have received endodontic therapy are typically advised to have cusp coverage with a crown restoration. Recent studies show that there is a correlation among the survival rate of endodontically treated teeth when restored with a crown. Anterior teeth with a conservative access cavity can be restored with a bonded restoration.
As you know- I’m always here to help you and your patients! Please reach out to me anytime at the office or via email: drjamie@cornerstoneendo.com
Until next time-
Jamie